Recognizing and Responding to an Opioid Overdose
Starseed Medicinal Sponsored Blog Post
Anyone who takes opioids can experience an overdose at any time. Examples of prescription or non-prescription opioids include fentanyl, oxycodone, hydrocodone, morphine, codeine and heroin.
When a person survives an opioid overdose, it’s because someone nearby understood an overdose was happening and how to take action. Call 911 immediately if you think someone is experiencing an opioid overdose.
When a person survives an opioid overdose, it’s because someone nearby understood an overdose was happening and how to take action. Call 911 immediately if you think someone is experiencing an opioid overdose.
Here's how to respond to an opioid overdose while waiting for emergency services:
How to recognize an overdose:
An opioid overdose happens when a person takes too much of an opioid, or a combination of opioids and other drugs, such as alcohol and benzodiazepines (like Xanax, Klonopin, Valium, Ativan, etc.) at a level that is toxic to the body, meaning it stops the body from working properly.
An opioid overdose happens when a person takes too much of an opioid, or a combination of opioids and other drugs, such as alcohol and benzodiazepines (like Xanax, Klonopin, Valium, Ativan, etc.) at a level that is toxic to the body, meaning it stops the body from working properly.
Sometimes it can be hard to tell if a person who is using opioids is just very high, or actually experiencing a life-threatening overdose. If you are unsure, it is best to assume there is an overdose — you could save a life.

Signs of an overdose include:
Unresponsiveness or unconsciousness.
Slowed or stopped breathing.
Snoring or gurgling sounds.
Cold or clammy skin.
Discoloured lips or fingernails.
Unresponsiveness or unconsciousness.
Slowed or stopped breathing.
Snoring or gurgling sounds.
Cold or clammy skin.
Discoloured lips or fingernails.
How to respond to an overdose:
1. Try to wake the person up.
Call their name or yell, "I'm going to call 911!" If they don't respond to your voice, rub the middle of their chest with your knuckles.
Call their name or yell, "I'm going to call 911!" If they don't respond to your voice, rub the middle of their chest with your knuckles.

2. Call 911 right away if you can't wake them up.
Follow the directions of the 911 operator. Tell the 911 operator if the person has slowed or stopped breathing.
The Law Is On Your Side
In Canada, the Good Samaritan Drug Overdose Act provides some legal protection for those who contact emergency services during an overdose. Those who are on the scene of an overdose when law enforcement arrives will not be charged with possession of a controlled substance. Check out our Opioids - What You Need To Know learning series for more information!

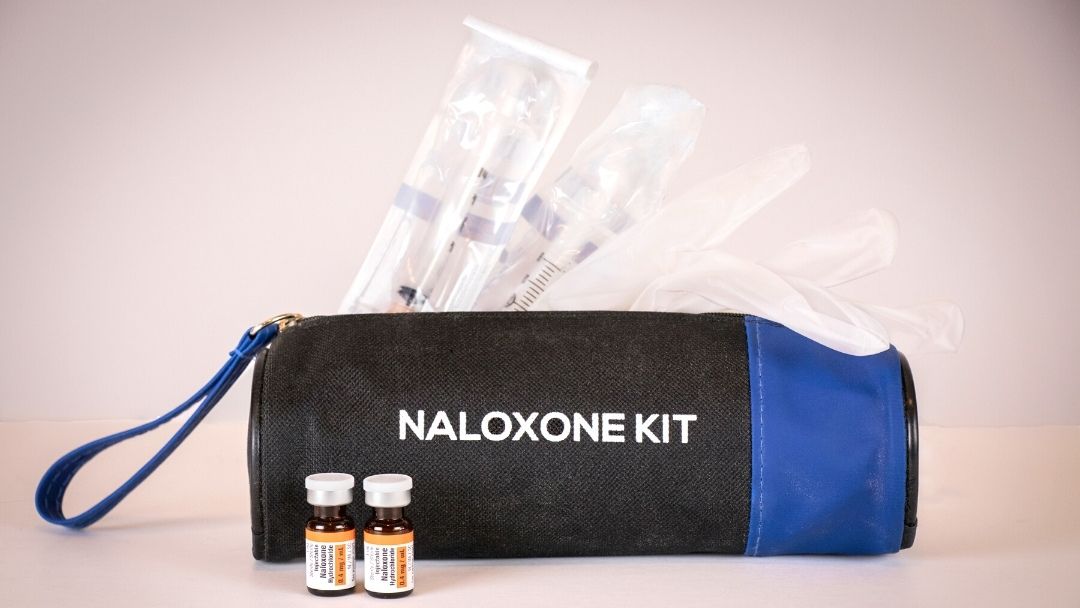
3. Give Naloxone if you have it.
If a person is not responding to noise, shaking of their shoulders or knuckles being rubbed on their sternum, and you suspect an overdose taking place, naloxone should be administered, right after calling emergency services.
Naloxone is a medication, also known as an “opioid antagonist,” that rapidly reverses and blocks the effects of an opioid overdose. If a person’s breathing has slowed or stopped due to an opioid overdose, Naloxone can quickly restore normal breathing. If a person does not have opioids in their system, then Naloxone has no effect. The medication is not a treatment for opioid use disorder. Find out where you can get free naloxone kits and training on how to use them through Ontario's Ministry of Health.
4. Start CPR (chest compressions) if trained to do so, and/or rescue breathing if the person's breath is slow or has stopped and it is safe to do so.
For CPR or compression-only CPR, follow your training or the instructions of the 911 operator.
For rescue breathing, make sure the person's mouth is not blocked, pinch their nose, and breathe into their mouth for 1 second watching for their chest to rise. After five seconds, administer another breath and continue rescue breathing. If there is no improvement after 2-3 minutes, administer Naloxone again and resume rescue efforts.
For rescue breathing, make sure the person's mouth is not blocked, pinch their nose, and breathe into their mouth for 1 second watching for their chest to rise. After five seconds, administer another breath and continue rescue breathing. If there is no improvement after 2-3 minutes, administer Naloxone again and resume rescue efforts.
Need help? Follow the directions of the 911 operator.

5. Put the person in the recovery position.
Once the person is breathing again, and if it is safe to do so or if you are instructed by the 911 operator, put them on their side with their top leg and arm crossed over the body to prevent choking. Stick around and keep an eye on the person until emergency help arrives.
For a full in-depth guide on recognizing and responding to an opioid overdose, download the CMHA guide.
More from our Blog

Empowering LiUNA workers and families with trusted education in health, wellness and workplace safety.
Copyright © 2025